Impact Report 2024/5
Creating a Healthier Somerset

Somerset was the first healthcare system in England to enter a formal partnership and alliance with voluntary, charitable, and third sector organisations to provide community mental healthcare services to patients across the county.
—Dr Andreas Papadopoulos, Somerset NHS Foundation Trust.
Our Impact in Numbers
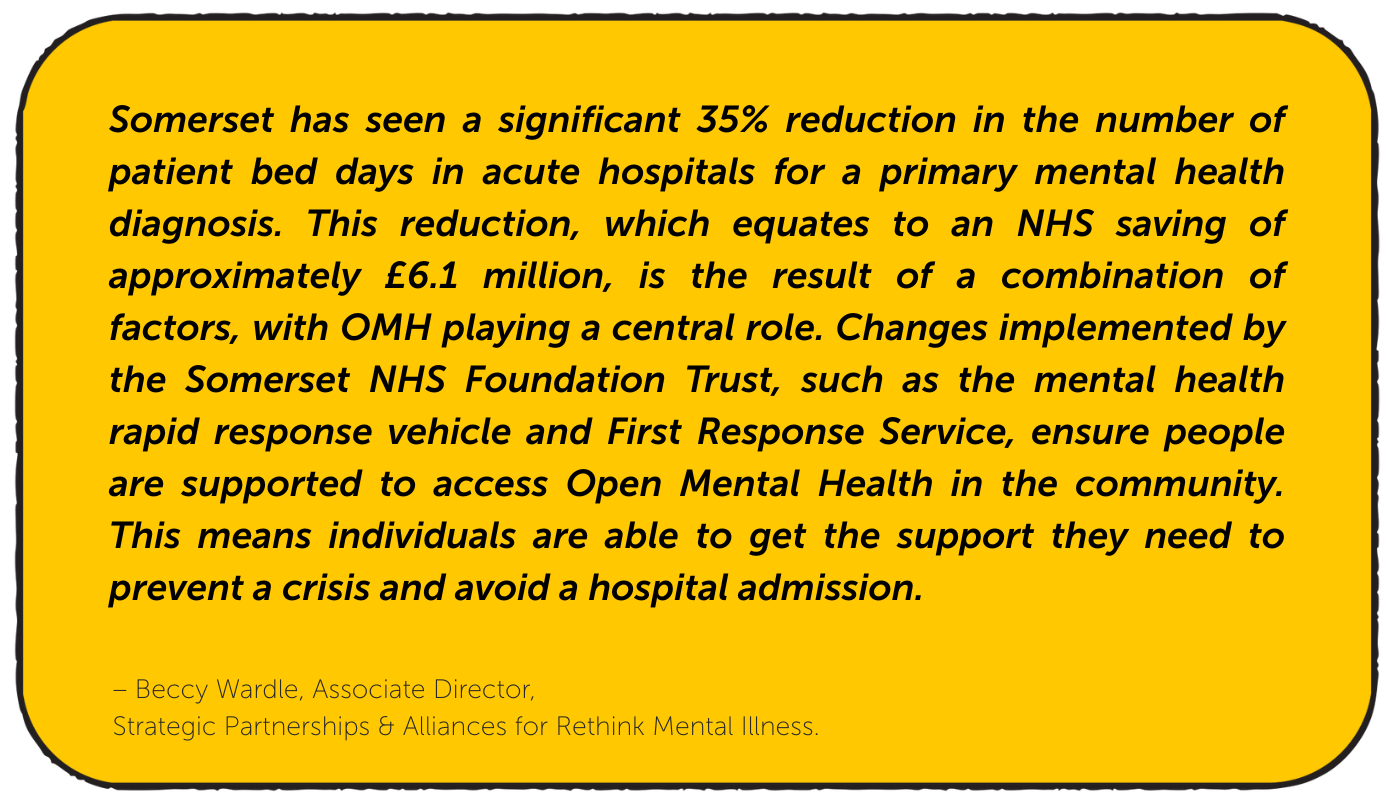
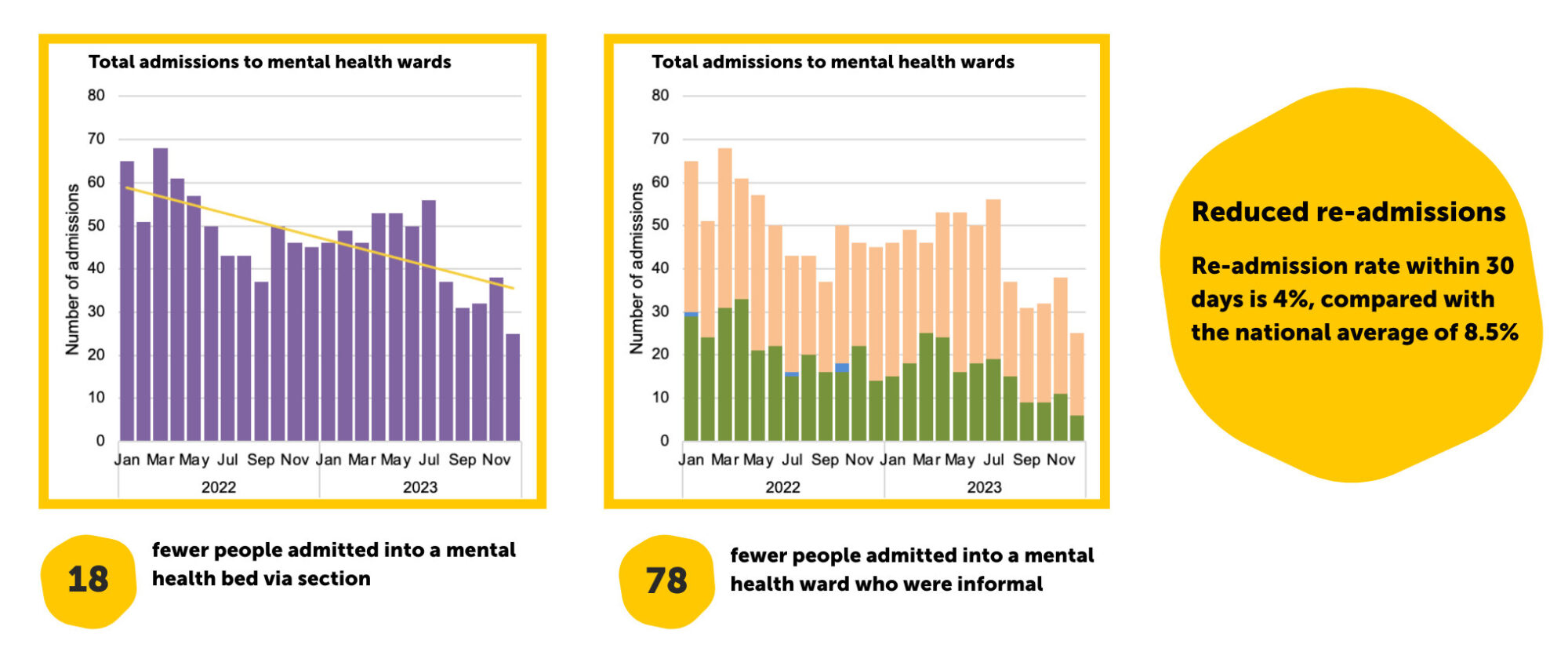
35% drop in number of bed days in an acute hospital – this number of bed days costs NHS approximately £6.1 million.
Interventions delivered in 2024-25.
Mental health re-admission rate is 4% – half the national average.
Mental health A&E attendances reduced by 15%.
Mental health inpatient admissions reduced by 18%.

Introduction
Our goal with this report is to share the journey we’ve been on in 2024-2025 and the difference our partnership made in the lives of people living with mental health challenges across Somerset.
Open Mental Health is an alliance of nineteen voluntary, community, faith, and social enterprises working in collaboration with the NHS and Somerset Council, and driven by the voice of lived experience.
We have a vision of achieving good mental health in Somerset through collective action. It’s our mission to deliver positive change by sharing our experience, expertise, and specialisms. We aim to grow and develop strong alliances across the voluntary, community, faith, and social enterprise sector to create a new way of working for mental health provision across Somerset, providing high-quality, reliable, joined-up, and effective services for everyone in all communities.

“In just a few years, Open Mental Health has grown from charity leaders’ shared vision of mental health support for everyone to a joined-up set of accessible services across Somerset. Guided throughout by experts by experience, watchwords like ‘no wrong door’ and ‘warm transfers’ have become a reality.
Underpinned by lead accountable body, Rethink, partnerships with Somerset Foundation NHS Trust, the Integrated Care Board, Somerset Council and the wider network of voluntary organisations have strengthened and deepened.
The numbers and personal accounts in this impact report do tell an inspiring story though it’s important not to overclaim and to retain due humility. There is still much to do to make sure that people can get the mental health support they need – where and when they need it most. Plans to improve outcome measurement, and draw on independent research, will help to identify gaps in provision as well as shedding more light on the contribution Open Mental Health makes 24/7 to the health and wellbeing of people across the county. There is tremendous scope to build on what has been achieved so far from preventative work to crisis safe support and recovery.
We want everyone to know that Open Mental Health is there for them.”
-Juliet Lyon CBE Co-Chair of Open Mental Health alliance

Working Together
Doing things differently and finding new solutions in Somerset
As an alliance, our collaborative approach provides people with resources to help them on their recovery journey, including specialised mental health services, housing and debt guidance, peer support, community activities, physical exercise, and wellbeing support.
Learning from each other, working together, and leading the way to become a stronger alliance and deliver positive change for everyone experiencing mental health challenges in Somerset. These are the core and associate partners in our alliance.


Doing things differently and finding new solutions in Somerset
“We are hugely grateful to everyone involved in OMH who welcomed us to Somerset and took the time to show and explain the fantastic collaborative work underway. What really came through was that your longstanding efforts to build and strengthen partnership working are already having a significant positive impact both for service users and frontline staff. We are looking forward to hearing more about the outcomes being achieved and how the learning from this innovative approach can support other local areas across England to provide more preventative, person-centred and proactive care. Many thanks to everyone involved in our visit.”
-Department of Health and Social Security.
Learn more about Somerset’s Winning Recipe for Mental Health
Online Wellbeing Toolkit
The 2024 Open Mental Health Festive Wellbeing Kit is an example of how pooling our resources empowers every member of our alliance to better serve the people of Somerset.
The kit offered mental health support targeted at the holiday period, which can be challenging, with pressures ranging from financial strain and isolation to societal expectations and social anxiety. With practical advice, resources, and tips from across the OMH alliance, the kit brought together knowledge and expertise to help keep people well and make the most of the festive period.
As our Experts by Experience explained: “…this resource is gold for peer support.”
We’re pleased to report that with the kit we created additional traffic to our website, letting people know about services is a top priority.
Extending our reach
- + 69.8% increase in reach on Facebook
- + 87.6% increase in active users to our website
(Based on data 1 Nov 24 – 1 Jan 25, compared to same period previous year)
By working together and bringing partners together we have pooled resources.

Experts by Experience
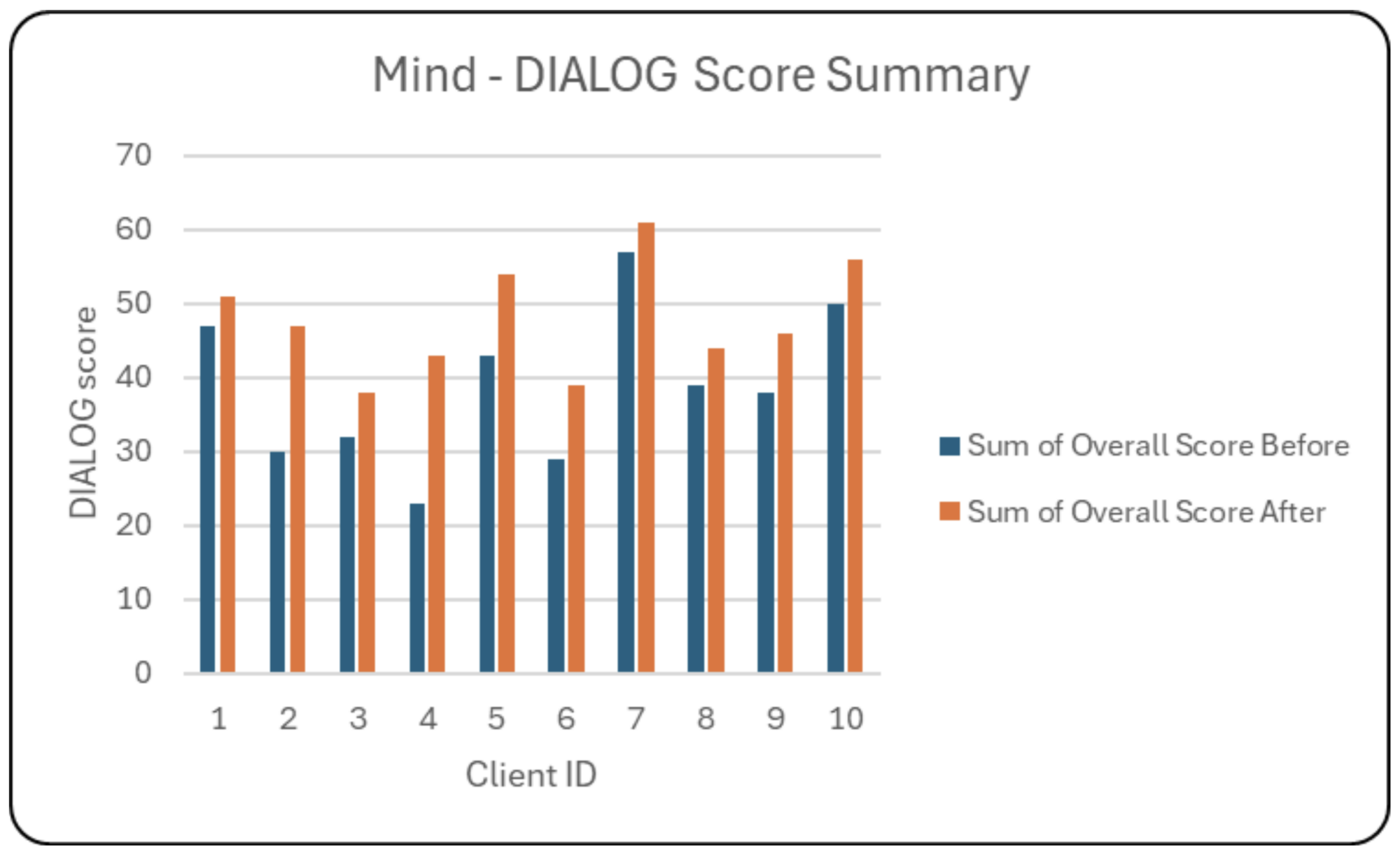
Experts by Experience are at the heart of OMH, working across a wide variety of projects and work groups. We’ve always believed in the power of co-production; it’s one of our core values. EbE leadership is essential to transforming Somerset’s mental health system. The benefits of experts by experience working collaboratively through co-production are clear: lived experience ensures services genuinely meet people’s needs and improve the quality of care for clients, carers, and their families.
EbEs contributed a total of 1755 hours of their time and hard-won knowledge.
(Financial year 24/25)
In 24/25, we had 9 Experts by Experience working across an average of 19 workstreams.
Expertise that Guides and Empowers
EbEs are involved in a wide variety of workstreams headed up by workstream leads who project manage. Our workstream leads consistently praise the impact our Experts by Experience have on OMH projects. Their involvement ensures our services are effective, relevant, and based on real-world needs.
OMH Locality Teams: Empowering Communities
Open Mental Health uses a locality model to ensure each individual receives the right care for their mental health within their own community. Our multidisciplinary teams in Taunton and West Somerset, Sedgemoor, South Somerset, and Mendip serve as community contact points for partnership working.
People seeking support are introduced to their locality team, made up of Recovery and Wellbeing Workers, a Locality Lead, and Locality Coordinator, who work with them to establish which services best address their needs.
Read some real-life stories of how the dedication of our Recovery and Wellbeing Workers transforms lives.
The teams offer more than just one-on-one help; they also deliver group sessions and courses, creating safe and friendly spaces for people to connect, learn new skills, and explore their interests alongside others.
South Somerset
An average of 40+ groups a month, with over 100 people attending a total of 250 interactions per month.
Taunton and West Somerset
2,454 session attendances
389 sessions delivered via 11 distinct groups.
Mendip
1067 session attendances,
187 sessions delivered via 5 distinct groups.
Sedgemoor
Delivered 3 groups a week including Coffee mornings, anger management and Understanding your Mental Health courses were held. Over 120 group sessions were delivered.
100% of people who completed the feedback form said they noticed an improvement in their mental health since attending a group session.
Our locality hubs & the work that they do
Groups & Courses
From January to May, the Sedgemoor team held 58 group sessions, supporting 174 people, offering an anger management course, an “understanding your mental health” course, and a regular coffee morning. 100% of people who completed the feedback form said they noticed an improvement in their mental health since attending a session.
“I feel a lot more confident and mentally better after speaking with the facilitators each week. It was a great help,” – course participant feedback.
In South Somerset, the team delivered an average of over 40 groups each month, reaching more than 100 people and resulting in 250 interactions every month, through Nature Connection Groups, a group for Autistic Adults, Chat Cafes in Wincanton and Crewkerne, a Men’s Group, and a Walk and Talk group.
The Mendip team’s community days at the Shepton Mallet Mind Hub are open to anyone over 18. Attendees have a safe and friendly space to try new activities, like art projects and nature-based sessions. Events are dog-friendly, so no one needs to miss out if they can’t leave their pet at home. The supportive environment encourages people to step out of their comfort zones.
“One client signed up for a cooking course at their local college, and they said they felt confident enough due to the skills they learned in one of the Open Mental Health cooking groups.” – Rebecca Richmond, Locality Lead
The Taunton and West Somerset team delivered 389 sessions to 11 distinct groups, accounting for 2,454 session attendances, and worked directly with the National Health Service:
“As well as delivering peer groups across the county, we worked with the inpatient unit in Taunton to jointly run a group session for individuals on the ward, with a view to sustainably supporting them back into the community.” – Charlie Acton-Pearce, Deputy Chief Operating Officer at Mind in Somerset
The team continues to deliver Hearing Voices training to the public through Somerset Skills and Learning, helping to reduce stigma and discrimination.

Real People – Changed Lives
Our locality teams support people from all walks of life facing a wide variety of challenges. Here are just a few of their stories, drawn from our life stories. Names have been changed to protect people’s identity.


Mindline Somerset 24/7
Mindline Somerset is a confidential, free, and non-judgemental listening service that offers a safe space for people to talk about their feelings and mental health struggles.
Mindline is a growing service, with 21% more calls answered from January to December 2024 compared to the previous year.
Mindline answered 44,485 calls in 2024-25.
3,040 of these were calls where the caller was at immediate risk of harm.
Mindline and NHS 111
In addition to the regular Mindline numbers, people in need can access the service by dialling 111 and choosing Option 2 for mental health support.
From April 2024 to March 2025, 3,644 calls were answered through this pathway from individuals experiencing suicidal feelings, thoughts, or intentions.

Crisis Safe Space
Crisis Safe Space gives out-of-hours support to Somerset residents, aged 18 or over, in emotional or psychological distress.

Interventions delivered in 2024-25
This is an increase of 11% compared to the same time scale 23/24.
Crisis Safe Space reduces pressure on the NHS. Clients say they would have used NHS services on 50% of occasions if it were not an option.
On 6% of occasions, clients reported they would have made a suicide attempt if Crisis Safe Space was not available.
1509 new clients were supported in 24/25 – an uplift of over 40% compared to the previous year.
This suggests we are reaching more new people and awareness of the service is increasing.
Open Mental Health Services

The Power of the Peer
Peer Support from WATCH CIO
74 clients introduced by OMH locality teams.
101 peer/volunteer training sessions delivered.
Peer Connections from Rethink.
Meet one of our peer mentors and discover more about the power of peer support >>
Disordered Eating
SWEDA delivers pro-recovery and empowering therapeutic support for people living with eating disorders. They also support caregivers and provide training for professionals.
In partnership with Mind in Somerset, SWEDA run dedicated eating disorders helpline for the people of Somerset on 0300 330 5464. The helpline is open every Sunday from 11am until 2pm and every Tuesday from 8pm until 11pm and offers free, impartial, confidential advice.
83% of clients at the end of their work with SWEDA reported an improvement in their eating disorder thoughts and behaviours.
Mel, a senior counsellor at SWEDA says that SWEDA collaborates with other OMH partners to ensure clients get the most appropriate support. If a client’s needs exceed SWEDA’s focus, they refer to or consult with organisations in the alliance. “We work very closely to make sure that we get people the right help,” she explains, adding that SWEDA liaise with OMH partners dealing with crisis, trauma, and other specific mental health issues.
On average the service is supporting 75 people per month.
80% of clients reported a reduction in physical distress.
237 referrals accepted.

Suicide Prevention
Peer Suicide Prevention Project
Delivered by Mind in Somerset and Second Step the project supports young adults aged 16 to 25 in Somerset. It’s a safe and supportive program for young people who are or have been at risk of self-harm and suicide, designed to help them talk openly about their feelings, connect with others, and find new ways to manage their mental health.
Wellbeing Mentors with lived experience of mental health challenges are available to guide young people, using their own journeys to provide support and reassurance. Through shared experiences and physical activity, they help to improve mental wellbeing, build social connections, and boost self-esteem, with the goal of helping young people feel more hopeful about their future.
The project on average supported 36 people per month across the service with 1000 appointments delivered to directly target people at high risk of suicide.
Our web page Understanding Suicide, a resource created in collaboration with our colleagues in the NHS for the Walk for a Life event, offers information for those affected by suicidal thoughts and their friends and families.
Recovery
Step Up – Rethink
The Step Up Service is a Crisis House in Yeovil that offers short-term accommodation for up to six people in a mental health crisis. Accepting county-wide referrals from the local NHS Home Treatment Service, it provided 1,143 occupied bed days. This effectively supported an average of 15 people per month, keeping them out of hospital and saving the equivalent of 1,143 hospital bed days.
Supported an average of 15 people per month.
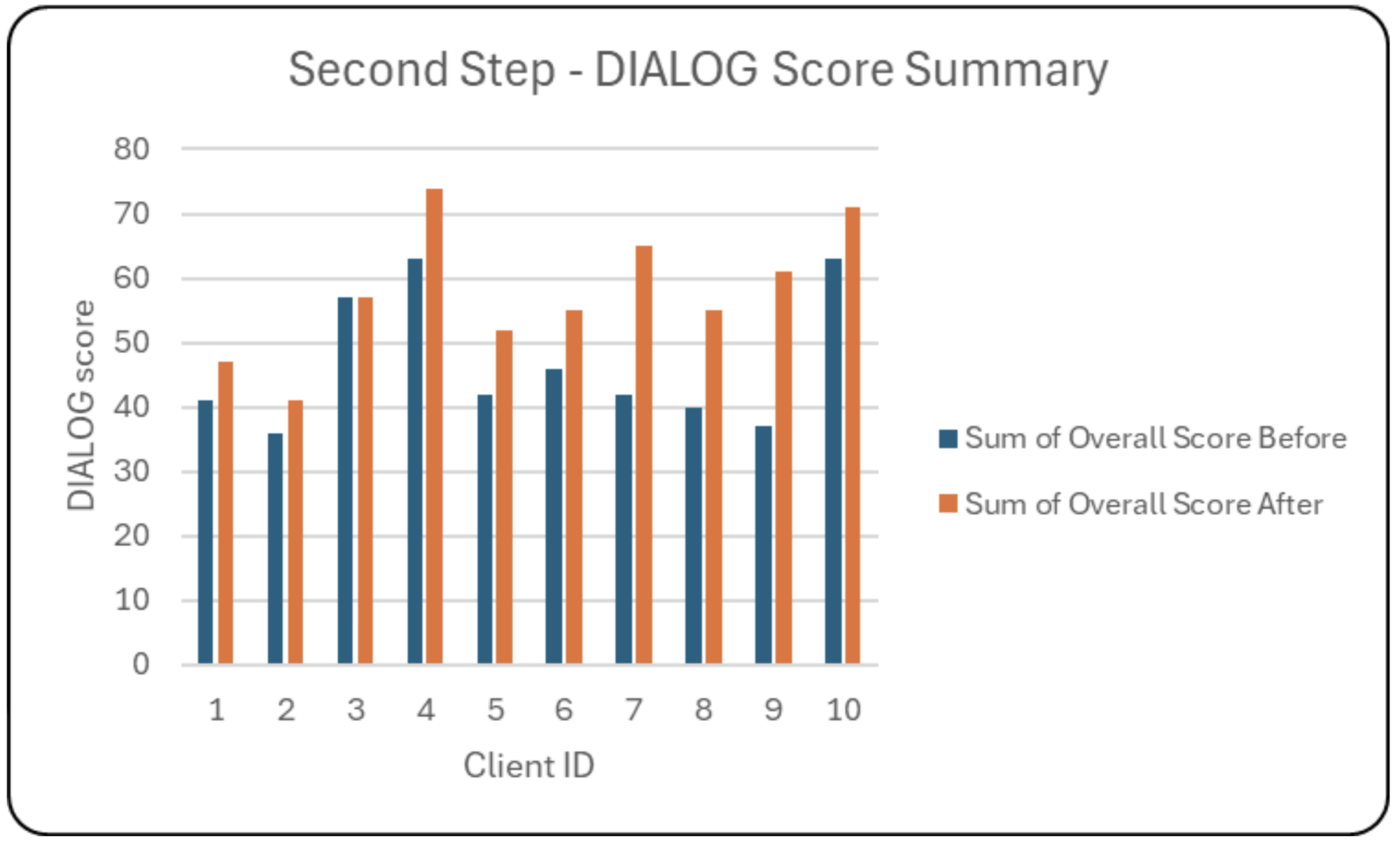
Step Down – Second Step
The Step Down service helps people transition back to community life after a stay in psychiatric inpatient care. The service uses a trauma-informed approach, ensuring that all support is tailored to each person’s unique experiences and needs. Out of 28 referrals received, 21 were accepted. The service supported 23 people across both its Yeovil and Wells locations, equating to 1,623 occupied bed days and freeing up NHS capacity.

Community Rehabilitation
Mental Health Community Rehabilitation workstream supports people with complex mental health difficulties to achieve their goals and gain skills and confidence to live as independently as possible.
The Rehabilitation Team is linked with key services across the county, including Open Mental Health, the Recovery College, and Somerset NHS Foundation Trust’s inpatient and community teams. There are also strong links to partner organisations outside the NHS, including housing and voluntary sector services.
From its inception, the Rehabilitation Team has been designed and shaped with the support of people with direct lived experience of coping with long-term mental health difficulties. Referrals and transfers to the service come from the NHS Trust only for the time being.
3250 interventions delivered via telephone, video conference or face to face.
An average of 18 people per month were supported to live an independent life in the community with aim of no return to MH ward.
Wider determinants of Mental Health
Staffed by a team of trained and qualified professionals who can provide advice on a variety of issues, Citizens Advice Somerset seeks to empower clients with the necessary knowledge and support to move forward, regardless of their circumstances or the nature of their problem.
Amongst other areas, Citizens Advice Somerset can help with:
Welfare benefits (including Universal Credit), Debt & Money, Housing, Family, Employment, Immigration, Discrimination, Food or fuel vouchers for those facing a crisis due to financial hardship
Citizens Advice Somerset delivered 2400 interventions.
(Jan-April 25)
This work helped 841 people resolve complex issues.
Caring for People
Friendly Phone Calls
Loneliness and social isolation can have a serious effect on older people’s health, and sadly, more than a million people over the age of 75 say they go a month or longer without speaking to a friend, neighbour or family member.
Thankfully, support is on hand in the form of Friendly Phone Calls. Anyone aged over 60 in Somerset feeling lonely, isolated, or low can have a telephone call from a friendly volunteer. Alongside the Walk and Talk and Wellbeing Friends programmes, Friendly Phone Calls is part of Open Mental Health partner Age UK Somerset’s Wellbeing Service.

On average, 175 older Somerset residents were supported each month either face to face or by phone.
The Carers Project delivered 186 interventions in 2024/2025.
Carers Project
Caring for someone with a mental health problem can be challenging, especially since a carer’s role often goes unrecognised. When people aren’t formally acknowledged as carers, their own emotional and practical needs can be overlooked, leaving them feeling isolated, exhausted, and unsure of what to do. The unfair stigma around mental health can make this harder, as some are too afraid of misconceptions to ask for the help they need. The Carers Project, led by Open Mental Health partner Thrive, assists people over 18 looking after someone struggling with their mental health in an unpaid caring capacity.
Families And Young People
The Family Safeguarding Team brings together mental health practitioners from Open Mental Health partners Mind in Somerset, Second Step and The Balsam Centre who are co-located within children’s social care teams. The team takes a trauma-informed, psychologically-informed approach to supporting parents whose mental health difficulties impact family life and safeguarding outcomes.
Practitioners provide structured, goal-focused interventions to help parents understand and manage their mental health, develop emotional regulation skills and strengthen family relationships. A Clinical Psychologist and Family Therapist from the voluntary sector provide consultation for complex families and hold a small caseload for more intensive support in high-risk cases, ensuring the team’s work is well supported and clinically guided.
2027 interventions were attended, 60% of which were face to face.

500 families supported across the county.

We’ve Got This
We’ve Got This provided young people across Somerset with peer mentoring to build self-esteem and confidence. Funded by Open Mental Health, it offered a fun and supportive environment where individuals can connect with others and feel more positive about their mental health.
Check out a life story or watch this video to discover more about We’ve Got This and the people the project supports.
945 interventions in financial year – 824 were one to one interventions.
We’ve Got This supported 82 young people across those 824 one to one interventions.
64 young people supported
82% improved their wellbeing score
68% accessed volunteering opportunities.
Peer Mentor Reported Outcomes
87% Positive Choices/Activities
59% Making Plans for the Future
72% Positive change in mental health and wellbeing
49% Better Self-Care.
Community Grants
Building on this success, we launched a new Small Grants Fund in 2025, in partnership with the Somerset Foundation Trust Charities Committee. This new fund distributed £100,000 among ten organisation to support smaller groups and enhance local community health and wellbeing.
We invite you to explore our 2023 Impact Report to see the impact of these grants firsthand. Discover hopeful and inspiring stories that show how the collective efforts of local people are making a real difference and shaping the future of mental health care across Somerset. Through the Open Mental Health grant fund, we are proud to empower smaller local charities in their great work.

£900K
awarded since 2020.
£218K
distributed in 2023 alone – supporting 26 community-led projects.
8,900
people supported through the programme in 2023.

Our Aspirations – where are we going?
Looking ahead, our strategy outlines a clear path for the future. These are our aspirations—the goals guiding our work to create a better mental health system for everyone in Somerset.

“We hope this impact report offered a window into the work and progress achieved by Open Mental Health, the people we’ve supported, the imaginative ways our teams have given support, and the impact of our joined-up approach across the community. We come from a variety of organisations, but we all share a common goal—improving the mental health and wellbeing of the people of Somerset. We believe that by working together as a collaborative alliance, we can make sure that everyone can access the right mental health support at the right time.“
– Jo Poole, OMH Co-Chair
Looking to the Future: A Model of Collaborative Care
“Having recently taken on my role as service group director, mental health and learning disabilities with Somerset NHS Foundation Trust, I’ve found it to be a very welcoming health and social care environment.
It was immediately apparent that everyone in Somerset, from colleagues in Open Mental Health to Somerset FT, and the wider system, has a real sense of positivity around how services are delivered, and how joint working contributes to that.
I’m constantly learning new and heart-warming things about the positive collaboration between Somerset FT and our voluntary sector partners in Open Mental Health.
The unique alliance model in Somerset is truly innovative and has rightly captured the attention of the rest of the country. I feel that the greatest strength of this approach is the principle of ‘no wrong door’.
Unlike the traditional approach, where limited resources often create barriers and ‘closed doors’, Open Mental Health ensures people can access support when they need it, before they reach a point of crisis.
This early intervention is the key to preventing the need for more acute care and helps to reduce the pressure on hospital services. It’s a truly accessible service, where patients don’t have to repeat their story multiple times.
The partnership embodies a ‘treatment to prevention’ shift that is absolutely fundamental to meeting the goals of the NHS 10-Year Plan, keeping care in the community where it belongs.
Moving forward, our aspiration is to build on this outstanding model. We need to ensure there is a clear and equitable offer across all four localities in Somerset, and that we keep working to improve our digital offer so it’s truly accessible to everyone.
Critically, we must strengthen our commitment to hearing the voice of people with lived experience. This includes listening to a wide cohort of patients and their families, using their feedback to continually improve and break down any remaining organisational barriers between the voluntary and statutory sectors.
We are committed to showing the long-term impact and benefit this alliance model has on people’s lives – because making a real difference to patient care is what it’s all about.”
—Mark Arruda-Bunker, Service Group Director, Mental Health and Learning Disabilities, Somerset NHS Foundation Trust.